Repair of the damaged spinal cord
How a clinical trial with a novel antibody brings new hope to people with a spinal cord injury and why Armin Curt has been dedicated to this extraordinary project for years. – An interview with Armin Curt, Professor of Paraplegiology at the University of Zurich.
There are about 250,000 people in Europe suffering from spinal cord injuries. What do these patients hope for?
For people with spinal cord injuries, the desire to find a cure and to recover never stops. Most of the patients find a way to adjust and live with the handicap, but heartfelt hopes do remain that there might be a cure one day. When you ask persons with a spinal cord injury what function they would like to get back if they could choose just one, walking is astonishingly not always mentioned. They ask for hand functions and bladder/sexual functions. Walking is of course a big desire but there are many other less recognised challenges as well.
What can these people hope for from the NISCI project?
The goal of the NISCI (Nogo Inhibition in Spinal Cord Injury) project is not to cure a complete paralysis. It is about finding first steps for a treatment to improve functions in the patients. Within this clinical trial, we focus on tetraplegic (quadriplegic) patients who suffer from an acute cervical injury (at the level of the neck), which results in an impairment of the legs but also of the arms and hands – a terrible condition indeed. About 50 percent of patients suffering from a spinal cord injury are tetraplegics (quadriplegics). In our clinical trial, patients will be administered a novel drug – the antibody against Nogo-A – to see how this modulates nerve function and hopefully improves the condition of the patients, specially the hand and arm functions. The trial is not a fishing expedition, we will not apply the drug and just see what may happen.
«This trial is not sponsored
by big pharma.
We even have to
roduce the drug.»
There are clear considerations as to what we look for, what we are going to test and what we expect. The trial is designed to answer a distinct question: How can we improve arm and hand functions? If you ask tetraplegic (quadriplegic) patients whether they prefer to be able to stand and walk or to use their hands, the patients will answer: Give me back my hands! I can live with a wheelchair but not being able to use my hands poses the greatest obstacles in terms of independence.
To what extent can you predict the degree of recovery of a spinal cord-injured person?
Within the European Multicenter Study about Spinal Cord Injuries Network (EMSCI), we have been developing and standardising recovery profiles for many years. Today, we have gathered the data of more than 4,000 patients within the network. Thanks to this data, we know the degree of recovery quite well that a patient with a specific spinal cord injury can achieve with the existing therapies and we also understand the timelines. Based on these data, we have developed prediction rules which work fairly well. So, when a patient comes to the hospital with an acute spinal cord injury, we can apply clinical test batteries and predict the likelihood for and degree of regaining arm/leg functions with the help of the existing therapies.
NISCI started in January 2016. What is the status of the project, two and a half years later?
We have set up the network, we have put together the protocol design and we have just handed in the applications for the trial to the regulatory bodies and ethics committees in Switzerland and the other EU countries involved in the project. Now we are close to the get-go and hope to start the clinical trial in September or October this year. The administrative efforts we have to manage are very demanding, they are on the highest level you can imagine, and it takes a great amount of time to pass all the regulatory hurdles. But we think it is worth to go through this lengthy and challenging process because it is about the safety of patients and, ultimately, we also must assure ourselves to be on solid ground.
When the trial starts in autumn, how will it be performed? How will you find the participating patients?
The great advantage of having this large European EMSCI network is that it includes experienced and dedicated SCI (spinal cord injury) centres that are dealing with this kind of patients. They are already trained to look at the patients in doing these assessments and we know what kind of patients they typically see and how many patients they treat per year.
«It is not about
writing nice papers,
it is about getting
our patients out
of the wheelchair.»
So, we cooperate with these centres to perform the clinical trial with their acute patients. Each of these centres will follow the same procedure. When new patients come in suffering from an acute spinal cord injury, they go through a checklist of inclusion and exclusion criteria and the data will be fed into a prediction calculator, which we share within the EMSCI network. When a patient enters the clinic either in Heidelberg or in Italy or wherever, he or she undergoes a standardised assessment and a prediction. And if the prediction indicates that after the conventional therapy he or she will end up with a very severe, disabling or a moderate impairment, we will invite this patient to enrol for the clinical trial.
What will then happen to the patient who agrees to enrol for the trial?
First, this patient undergoes various standardised and basic clinical tests as well as some additional advanced assessments based on the protocol of the study. This test battery has been trained by the centres. They do them already now, on their regular patients. These are clinical tests on what the patient can feel, how he can move, there are imaging tests of the spine from which you see how the spinal cord looks like, where exactly the lesion is located and how grave it is. There will also be some measurements of nerves fibres of arms and legs. All these data will be the base for the enrolment of the patient.
And how will the drug then be administered?
The antibody will be injected into the cerebrospinal fluid (CFS) compartment at the lumbar backbone of the patient. It is a typical CSF punch, which you also do when you are looking for meningitis or any inflammation in the CSF. The injection, the dosing, the time interval is exactly the same as we did already in the phase 1 study from 2006 to 2008.
«My dream is to see
the first approach
that truly helps to repair
the damaged spinal cord
and make it recover.»
This was a study on safety and feasibility from which we learned that the drug has no negative impact on the patient and the way of application has been proven to be safe. Based on the results of this phase 1 study, we will do the clinical trial now in phase 2. There will be six injections within four weeks after the injury, when the nervous system is still plastic enough, allowing to obtain some improvements or increase plasticity. The patient will then be guarded for six months to evaluate the result. The procedure will be exactly the same in each centre. The physicians and nurses performing the trial on site are trained to apply the drug and deal with the patient. But here comes the difficult point. This is a randomised controlled double-blind study, the highest level you can have. Hence, when I treat a patient here in Zurich, I do not know if I am going to inject the drug or just a placebo. Only after a while we can unblind the study and see which one did better, the drug or the placebo.
Half of the patients participating in the trial receive the drugs and may benefit. But the other half receive a placebo and miss a possible improvement. How do you deal with this ethical challenge?
This has been a fundamental problem ever since there have been clinical trials. And to be honest, it is also a challenge for us. But for the rigour of a trial, this is exactly what is needed. All these approval studies are typically designed in this double-blind pattern with placebo and real treatment. There is no way yet on this level of drug development to overcome this challenge. It is an unsolved problem. But it is important to understand that if you have novel drug treatments that are applied for the first time to humans, you must acquire truly valuable clinical data. It cannot be imprecise, as afterwards you may treat thousands of people. When you start with a design flaw and flawed outcomes, this will affect the other thousands of patients to follow. It is a difficult topic.
What is the other main challenge you are facing within this project?
First of all, this is an investigator-initiated trial (IIT), meaning this trial is not sponsored by big pharma. The University of Zurich is the main sponsor. We have co-funding from the EU (Horizon 2020) and the Wyss Zurich is also involved. We even have to produce the drug. This process to produce and get the antibody ready for application is an enormous effort, steered and managed by Martin Schwab and his group at the Wyss Zurich and the University of Zurich. It’s a great challenge. That is one part. The other part is that this is a multinational trial including at least twelve centres and I as the clinical PI have to shepherd all these centres and people into the same direction. Moreover, I also have to look for additional funding. We have the EU funding, which covers about 75 percent of the costs. We also gained funding from the Swiss Paraplegics Association and from Wings for Life in Austria. But I have to make sure that we are not running out of fuel. The NISCI project is a very ambitious undertaking that only works because we have a very good setup here at Balgrist with people in clinical care, SCI research as well as experienced study nurses and many others to help. It is not a one-man show, it is truly a big, big team effort.
You are very experienced in coordinating complex translational projects. What does this NISCI project mean to you?
The concept of neuroplasticity and the concept to overcome the inhibition that blocks the regeneration of injured fibre tracts in the central nervous system has been pioneered here in Zurich and has a long exciting tradition to work on. After such a long journey, we definitely want to see now if this is really able to change the outcome for our patients. I am a clinician, I see patients on a daily basis and I feel with my patients.
If you ask tetraplegic patients
whether they prefer
to be able to walk
or use their hands,
they answer:
Give me back my hands!
I want to see a change. Having all these experiences with this antibody approach and all these preclinical studies, we would like to witness it in humans. Hence, we have a very strong interest to observe this based on the scientific background but also on a day-to-day basis when we treat our patients. It is not about writing nice papers, it is about getting our patients out of the wheelchair. Therefore, we have a strong desire to do something. This clinical trial offers very special conditions. We had other trials with stem cells, with robotics; they all had their special ideas and approaches. However, having the first drug to allow the nervous system (i.e. spinal cord) to be more plastic and achieve an improvement of functions – that is what we would like to have.
Is there realistic hope that a patient steps out of the wheelchair after the use of this drug?
Based on my experience, this is very unlikely. There are no miracles. Currently, we do this trial with acute patients to see whether this approach has the potential to improve plasticity and might potentially help our patients. Nevertheless, we also intend to test it eventually on chronic patients who suffer from the result of a spinal cord injury. There are more chronic than acute patients. First, however, we need to establish this treatment, showing its worth and open the field to further exploration and investment. Another big challenge is the fact that big pharma has shied away from this extremely difficult field so far. They can earn money more easily with other projects and larger recipient numbers. But we would like to prove that there is reason enough to invest in this treatment.
What would be your dream?
My dream is to find the first treatment to improve the neurological recovery after a spinal cord injury. By today there is simply no treatment available to repair the damaged cord. We can offer rehabilitation around the damaged cord. So far, this is the only proven treatment to help the patients, and the existing rehabilitation interventions have a good impact on their lives. But obviously they are still limited. I have always wondered why this silly spinal cord refuses to recover (laughing). So, I would like to see the first approach that truly helps to repair the damaged spinal cord and make it recover.
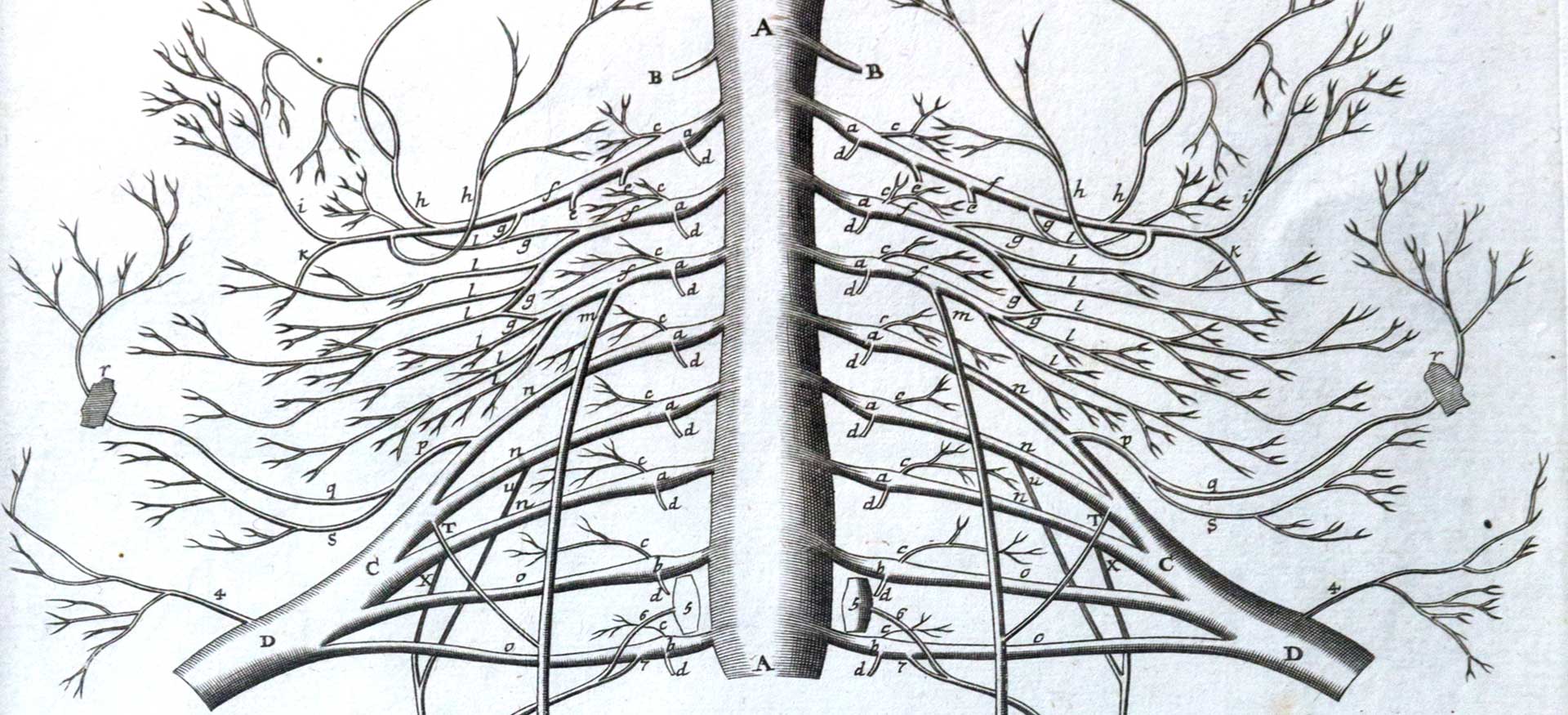
The long way from basic research to a novel therapy
Injured nerves in the human body are able to regenerate and regrow. But there is one terrible exception: The fibres of the central nervous system of the spinal cord. Therefore, people suffering from a spinal cord injury are partly or fully paralysed for the rest of their lives. Up to now, there is no therapy that repairs the damaged spinal cord nerves. In 1985, Martin Schwab, Professor of Neuroscience at the University of Zurich (since 1985) and ETH Zurich (since 1997) postulated the concept of «inhibitors of neurite growth» as a cause of the absent regeneration of injured fibre tracts in the central nervous system. Subsequently, he isolated one of the most potent nerve fibre growth inhibitors, a protein called Nogo-A. When this protein was blocked, regeneration and functional repair could be shown for the first time in adult rats and monkeys after spinal cord injuries. In a next step, Martin Schwab and his team developed an antibody against Nogo-A which was tested in trials with animals in the early 2000s. The first trial in human beings (2006 – 2008) proved that the antibody is safe and tolerable. In autumn 2018, a second clinical proof of concept trial will start with 140 acute patients suffering from a spinal cord injury to test the efficacy of this antibody therapy. After 33 years of research and trials, there is hope to develop a therapy that helps to repair the damaged spinal cord nerves and make them recover.
Interview with Armin Curt
Armin Curt
Armin Curt has been Professor for Paraplegiology at the University of Zurich and Medical Director of the Spinal Cord Injury Centre at Balgrist University Hospital Zurich since 2009. In 1987, he received his medical degree at the University of Cologne, Germany. After postdoctoral studies in Neurology and Psychiatry in Cologne and Zurich, he joined the Spinal Cord Injury Centre at Balgrist University Hospital, where he specialised in Paraplegiology. From 2005 to 2008, he was Associate Professor in Neurology and SCI Research at the University of British Columbia at Vancouver, Canada. Armin Curt is highly interested and engaged in translational work, bridging basic research and daily clinical practice.
Project funded by Horizon 2020
«NISCI – Antibodies against Nogo-A to enhance plasticity, regeneration and functional recovery after acute spinal cord injury, a multicenter European clinical proof of concept trial», Collaborative Research and Innovation Action
- Duration: 2016-2020
- Coordinator: University of Zurich, Switzerland
- Partners: 11 partners from 6 different countries
- Financial contribution from H2020: 4,774,444 €
(1,928,534 € for University of Zurich)